Addiction has long been viewed through lenses of morality, willpower, or flawed character. However, modern neuroscience paints a different picture—addiction is a chronic brain disease marked by alterations in brain circuitry, especially in areas responsible for reward, impulse control, and decision-making. This understanding has opened the door to innovative treatment methods that directly target the brain. Among the most promising are neurotherapies—cutting-edge interventions that aim to rewire the brain and support lasting recovery.
Understanding Addiction as a Brain Disease
To appreciate how neurotherapies work, it’s essential to understand addiction at the neurological level. Substances like alcohol, opioids, and stimulants hijack the brain’s reward system, flooding it with dopamine and reinforcing behaviors that lead to continued use. Over time, repeated substance use leads to structural and functional changes in the brain, particularly in the prefrontal cortex (which governs judgment and self-control) and the limbic system (which regulates emotions and rewards).
These changes create a vicious cycle of craving and compulsive use, making it extremely difficult to stop without intervention—even when the person genuinely wants to recover.
Enter Neurotherapies: Reprogramming the Brain
Neurotherapies represent a new frontier in treating substance use disorders. Rather than focusing solely on behavioral interventions or pharmaceutical aids, these therapies work to restore healthy brain function through technological and neurobiological methods. While they are not magic bullets, they can enhance traditional treatment approaches and help prevent relapse.
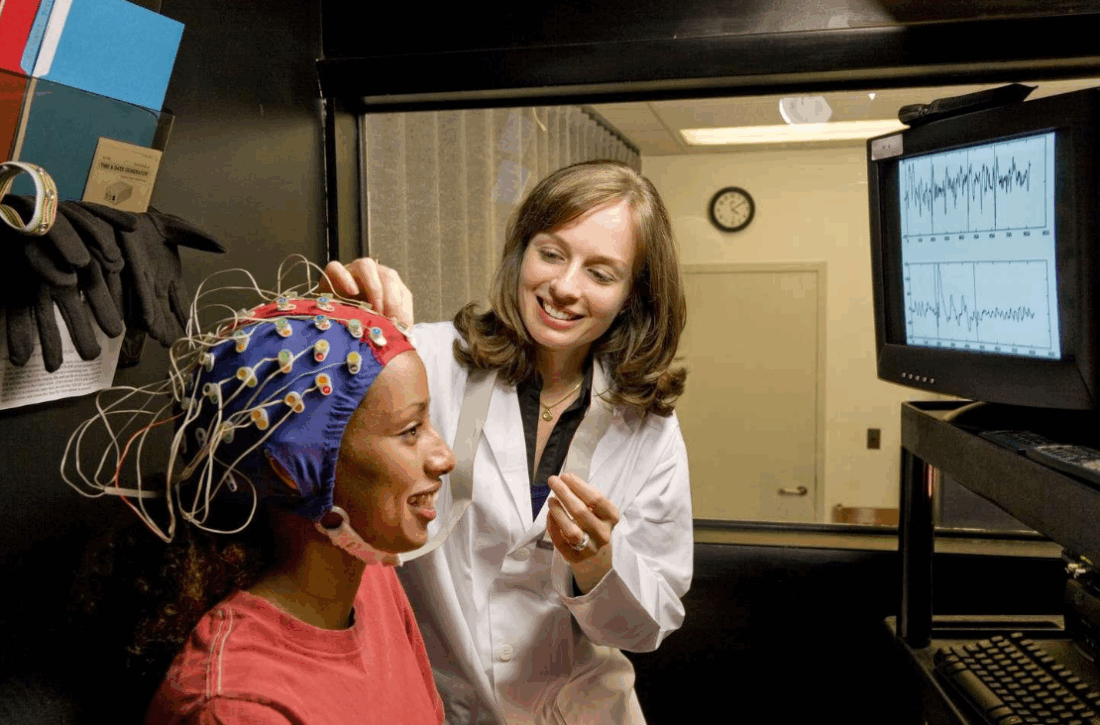
1. Neurofeedback (EEG Biofeedback)
Neurofeedback is a non-invasive technique that teaches individuals to regulate their own brain activity. Using sensors placed on the scalp, real-time brainwave patterns are displayed on a screen. The individual performs mental tasks or receives feedback (such as visual or audio cues) when their brain reaches a desirable state.
Over time, this “training” encourages the brain to shift away from maladaptive patterns associated with addiction—like excessive theta or beta waves linked to impulsivity and cravings—and move toward healthier functioning. Neurofeedback has shown promise in treating alcohol, opioid, and stimulant dependencies, often improving attention, mood, and impulse control.
2. Transcranial Magnetic Stimulation (TMS)
TMS uses magnetic fields to stimulate specific regions of the brain, particularly the prefrontal cortex. In individuals with addiction, this area tends to be underactive, contributing to poor decision-making and inability to resist cravings.
During a TMS session, a coil placed against the scalp sends brief magnetic pulses to the brain. Research shows that repeated sessions can restore executive function and reduce cravings by modulating dopamine pathways. TMS is FDA-approved for depression and is increasingly being investigated for addiction, especially to nicotine, cocaine, and alcohol.
3. Transcranial Direct Current Stimulation (tDCS)
tDCS is another form of brain stimulation, but unlike TMS, it uses a weak electrical current rather than magnetic pulses. Electrodes are placed on the scalp to target specific brain regions and modify neural excitability.
Studies suggest that tDCS can reduce substance cravings and improve cognitive control, especially when combined with behavioral therapy. It’s less expensive and more portable than TMS, though more research is needed to standardize protocols and verify long-term effects.
4. Cognitive Remediation Therapy (CRT)
Addiction often impairs attention, memory, and executive function. CRT is a form of therapy that uses structured mental exercises—often delivered via computer programs—to improve these cognitive domains. Think of it as a brain gym.
While not a neurotherapy in the traditional sense (it doesn’t involve electrical or magnetic stimulation), CRT plays a crucial role in rewiring neural pathways. When integrated with other neurotherapies, it can accelerate recovery and increase treatment retention.
5. Deep Brain Stimulation (DBS)
DBS is an invasive but highly targeted treatment involving the surgical implantation of electrodes into specific areas of the brain. These electrodes deliver controlled electrical impulses to modulate brain activity.
Though primarily used for movement disorders like Parkinson’s disease, DBS has shown early promise in treating severe, treatment-resistant cases of addiction, particularly opioid and alcohol dependence. Because of its risks and costs, DBS is typically reserved for clinical trials or experimental therapies.
Benefits of Neurotherapies in Addiction Treatment
Neurotherapies offer several advantages that make them appealing adjuncts to traditional addiction treatment:
- Non-pharmacological: They avoid the risk of substituting one drug for another.
- Targeted intervention: These therapies can focus on specific brain regions and circuits.
- Personalized treatment: Brain-based diagnostics can tailor interventions to the individual.
- Low side-effect profile: Most non-invasive therapies are well-tolerated with minimal risks.
Integrating Neurotherapies Into Holistic Recovery
It’s important to note that neurotherapies are not standalone cures. Addiction is a multifaceted condition with psychological, social, and environmental components. The most effective treatment plans incorporate neurotherapies alongside:
- Cognitive-behavioral therapy (CBT)
- Motivational interviewing
- Support groups (e.g., 12-step programs)
- Family counseling
- Nutritional and physical wellness programs
When combined, these approaches offer a comprehensive path toward healing and recovery.
Limitations and Considerations
Despite their potential, neurotherapies also come with limitations:
- Access and affordability: Equipment and trained professionals are not widely available in all regions.
- Limited long-term data: While early studies are promising, more research is needed to confirm sustained benefits.
- Variability in outcomes: Not all individuals respond equally to neurotherapy, and treatment must be individualized.
Nevertheless, with growing evidence and technological advancement, neurotherapies are rapidly moving from experimental to essential components of modern addiction treatment.
The Future of Brain-Based Recovery
As science deepens its understanding of the brain, the future of addiction treatment will likely involve even more sophisticated neurotechnologies. Possibilities include:
- AI-driven neurofeedback systems for adaptive learning
- Wearable neurostimulation devices for on-demand craving control
- Personalized brain mapping to guide therapy choices
- Real-time monitoring of brain activity during recovery phases
This future envisions not only better outcomes but also greater compassion—replacing stigma with science, and punishment with personalized care.
Final Thoughts
Addiction alters the brain, but the brain is capable of change. Neurotherapies represent a hopeful advance in the journey of recovery—one that respects both the complexity of addiction and the incredible resilience of the human mind. By literally rewiring the brain, these therapies empower individuals not just to recover, but to thrive.