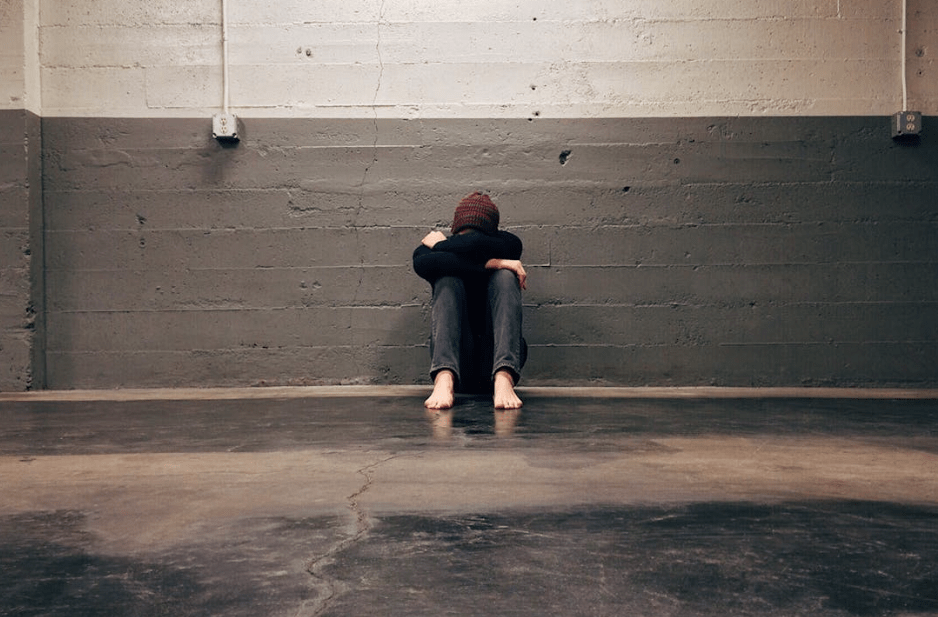
When a teenager begins to show signs of depression, the experience can be confusing, painful, and overwhelming for the entire family.
As a parent or caregiver, the core question you likely have is simple but urgent: What are the treatment options for my teen struggling with depression?
The good news is that there are many effective, evidence-based approaches available, and with early intervention, the prognosis for teens with depression is generally positive.
In this article, The Bragging Mommy will walk you through the main treatment options available to adolescents facing depression, from therapy to medication, and from outpatient care to residential programs.
Along the way, we’ll answer common questions parents have, unpack how treatment is tailored to individual needs, and explore emerging strategies that help teens not only stabilize but truly thrive.
Understanding Teen Depression: A Brief Overview
Before diving into treatment, it’s helpful to understand how depression shows up in teens. While sadness is a normal part of adolescence, clinical depression is more persistent and pervasive.
It can affect a teen’s mood, sleep, appetite, self-worth, relationships, academic performance, and motivation. Symptoms can vary significantly from one teen to another and may include irritability, fatigue, social withdrawal, feelings of hopelessness, or even self-harming behaviors.
Teen depression is treatable—but it often requires a comprehensive approach tailored to each young person’s emotional, developmental, and environmental context. You can also consider understanding what are Spravato treatments.
Starting the Process: Evaluation and Diagnosis
The first step in finding the right treatment is getting a thorough clinical evaluation by a licensed mental health professional. This can be initiated through your child’s pediatrician, a school counselor, or a therapist with experience in adolescent mental health.
A complete assessment typically includes:
- A diagnostic interview with the teen
- Conversations with caregivers or teachers to gain additional insight
- Screening tools and questionnaires
- A review of medical history and current stressors
Accurate diagnosis is essential to determine whether your teen is experiencing major depressive disorder, dysthymia (persistent depressive disorder), bipolar disorder, or another condition that may require a specific course of care.
Outpatient Depression Therapy for Teens: The First Line of Treatment
For many teens, outpatient therapy is the most appropriate starting point. This level of care allows them to maintain school and family routines while receiving consistent mental health support.
Cognitive Behavioral Therapy (CBT) is one of the most widely recommended approaches. It helps teens identify negative thought patterns, develop coping skills, and engage in behavioral changes that support mood regulation.
Dialectical Behavior Therapy (DBT), originally developed for individuals with intense emotional experiences, is also commonly used with teens, especially those exhibiting self-harm or suicidal ideation.
Therapy sessions may be individual, family-based, or a combination of both. Family involvement is often crucial, as teens recover more effectively when their home environment is supportive and well-informed.
Group Therapy and School-Based Supports for Adolescent Depression
Adolescents often respond well to group therapy, where they can connect with peers facing similar challenges. These groups are typically led by a licensed therapist and focus on skill-building, communication, emotional regulation, and peer support.
Many schools now offer school-based counseling services, which provide teens with access to therapists or psychologists during school hours. While these services may be limited in scope, they can be a helpful supplement to outpatient care and a vital connection to mental health resources.
Psychiatric Medication for Depressed Teens: When Is It Appropriate?
Parents often wonder whether antidepressants are necessary—or even safe—for teenagers. While medication isn’t always needed, it can play a valuable role in treatment for moderate to severe depression, especially when therapy alone is not enough.
Selective Serotonin Reuptake Inhibitors (SSRIs), such as fluoxetine (Prozac), are commonly prescribed to adolescents and are FDA-approved for this age group. The decision to start medication should always involve careful discussion between the prescriber, the teen, and the family.
It’s important to monitor for side effects and ensure regular follow-ups during the initial months of use.
Medication is most effective when paired with ongoing therapy. It should never be a stand-alone treatment unless advised by a qualified psychiatric provider.
Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP)
When depression symptoms become more severe or begin to disrupt a teen’s ability to function in school or at home, Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP) may be appropriate.
These structured programs provide several hours of therapeutic support multiple days per week. They are ideal for teens who need more support than traditional outpatient therapy can provide but who do not require 24/7 care.
IOPs and PHPs often include:
- Individual and group therapy
- Family therapy sessions
- Medication management
- Academic support or coordination with schools
- Structured daily routines
These programs are a middle ground that allow teens to receive focused care while still living at home and participating in family life.
Residential Treatment: When 24/7 Care Is Needed for Your Teen
If your teen’s depression has become unmanageable at home or includes serious risks such as suicidal behavior, self-harm, or co-occurring disorders, residential treatment may be the safest and most effective option.
These programs offer 24-hour care in a therapeutic, supportive setting and are designed to help teens stabilize and begin deeper work on the underlying causes of their depression. Treatment includes:
- Daily therapy and psychiatric care
- Educational support to stay on track with school
- Recreational therapy and life skills development
- Family therapy and parent workshops
- Aftercare planning for a successful return home
Choosing an accredited teen program in Tucson, or elsewhere, ensures that the care your teen receives meets established clinical and safety standards.
Specialized Programs for Co-Occurring Conditions
Many teens with depression also struggle with other mental health issues such as anxiety, trauma, ADHD, or substance use. In these cases, treatment must address the full spectrum of your child’s needs.
Evidence-based programs for depressed teenagers often incorporate trauma-informed care, substance use counseling, and neurodevelopmental assessments to create a holistic and personalized plan.
Supporting Recovery at Home for Teens With Depression
Regardless of the level of care your teen receives, your involvement as a parent or caregiver is vital. You don’t need to have all the answers—but showing up, staying engaged, and learning alongside your teen makes a big difference.
Consider the following at-home strategies:
- Maintain open, non-judgmental communication
- Encourage consistent sleep, nutrition, and exercise
- Limit screen time and promote real-life connections
- Attend family therapy or parent support groups
- Monitor progress and stay involved in aftercare planning
Recovery from depression is not linear. Your teen may have good days and bad days—but with the right support system in place, they can regain hope, motivation, and resilience.
For example, if your teen’s depression is linked to past trauma, they may benefit from treatment options for teens with PTSD, such as EMDR (Eye Movement Desensitization and Reprocessing), trauma-focused CBT, or somatic therapies that help the body release stored stress.
A Message of Hope for Parents of Teens Struggling with Depression
If you’re reading this because you’re concerned about your child, please know this: you’re not alone, and there is help available. While it can be daunting to navigate treatment options, every step you take brings your teen closer to healing. The path forward may require trial and error, but it is built on proven practices and the powerful bond between you and your child.
Depression doesn’t have to define your teen’s future. With the right combination of clinical support, compassionate care, and family involvement, your teen can move from surviving to truly thriving.
If you’re unsure where to start, reach out to a licensed mental health provider in your area who specializes in adolescent care. Early intervention can be life-changing—and even life-saving.